The highly transmissible P.1 variant of SARS-CoV-2 first appeared in the U.S. in Minnesota, and it was the Minnesota Public Health Laboratory, where Dr. Sean Wang works, which discovered it.
Like so many other things about this year with COVID-19, news of the arrival of P.1 came at an inconvenient time: it was a Monday morning in late January and Dr. Wang, head of the sequencing and bioinformatics unit in the infectious disease lab section of the Minnesota Department of Health, got the message from his staff when he was just about to hop onto a commuter train in Minneapolis so he could get his first COVID-19 vaccine shot.
“There is another thing: We found a P.1,” he recalled the staff writing him. “I was like, wait, are you serious? And my staff was like, yes.”
This was unwanted news, but not entirely unexpected. As he boarded the train, Dr. Wang instructed staff to put in place their existing protocols to deal with just such a situation: Make sure the data were authentic, do a separate individual analysis to confirm that the variant was P.1, manually examine each amino acid mutation to make sure they were not missing anything, and immediately reach out to his epidemiology colleague at the department to start gathering background and assessing the impact.
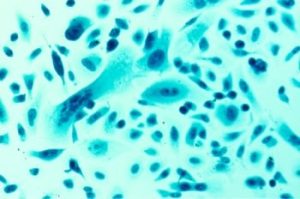
Epidemiology pulled through—the individual who returned the P.1 diagnosis had recently come back from the Manaus, Brazil region. Manaus is a jungle capital deep in the heart of the Amazon and ground zero for the so-called Brazilian mutation of SARS-CoV-2, which has shown to spread much faster than other variants. After Minnesota’s first P.1 reporting, there are now at least 61 cases reported from 18 jurisdictions.
What was interesting, Wang said later, was that his team was not necessarily looking for P.1. Since SARS-CoV-2 landed in America last year, Wang’s lab has been fully devoted to sequencing samples of the virus.
“This was found in literally a random sample,” he said.
But the finding also highlighted the unique ways labs like Wang’s have partnered with various agencies both locally and around the nation.
“Knowing the person had recently traveled to Brazil and returned, that really helped to increase our confidence in terms of our data since this is the very first sequencing-confirmed P.1 case in the United States” he said. Lab staff, he said, checked the mutations and redid bioinformatics analyses to confirm that the variant they were looking at was P.1, but it was the epidemiological background that gave them the final boost of confidence, enough to escalate the situation and get others involved.
Wang’s lab has been deep into whole genome sequencing since 2014, but before the pandemic began, staff were mostly focused on sequencing the genomes of things like bacteria, salmonella, E. coli, strep, and different bacterial pathogens and fungi. But that came almost to a halt the moment the state saw its first COVID-19 diagnosis, which happened on March 6, 2020.
“We had some limited experience with viruses, but this was the first time we used this style of sequencing,” he said. “But it was not hugely technically difficult because we already had experience with sequencing in bioinformatics.”
For SARS-CoV-2, Wang’s lab uses ARTIC primer sets—they are now using the V3 updated amplicon set. The lab’s first primers were shared by the public health lab in Utah, Dr. Wang explained. The Minnesota lab had ordered a set of primers but they were not in hand yet, and a colleague helped him out by shipping a small amount of material that ended up being key. Currently, the Minnesota lab is running about 450 samples weekly compared to last year’s 90 samples per week.
In the early days of the pandemic, Wang’s department was heavily focused on genomic baselines for the disease to get a broader picture of what was happening in Minnesota. After a couple of months, the focus shifted to epidemiology and clinical partnerships to investigate outbreaks—deep dives into virus clusters in long-term care facilities, correction facilities, meat processing plants, and among those who had attended outdoor concerts, events, and restaurants.
“That helped us to really have the anatomy of outbreaks using whole genome sequencing,” he said. “And that is still ongoing.”
The lab is also testing random specimens from all over the state to track mutations while creating parallel teams with epidemiologists to investigate possible reinfections.
“I am grateful to have support from the executive level, that they had confidence in us to keep up with the sequencing work,” Wang added. “It was a hunch at the beginning that we should get this sequencing thing going, though back then it was all hands on deck with the entire lab doing COVID testing. It takes a lot to keep that going for a number of months.”
Alliances like the one with Utah have been key, Wang said. Currently, StaPH-B (State Public Health Bioinformatic) group, which Dr. Sean co-founded with his counterparts at state public health labs of three other states—Colorado, Utah, and Virginia—serves as the information exchange hub. There are multiple levels of collaboration, ranging from GitHub to a Slack channel to a monthly webinar with a subscriber list that just keeps on growing.
“If I have a question,” he said, “I post it. And someone always answers it. People think of science as being very regimented and top-down, but scientists love to work with each other.”
That particular alliance is indicative of one of the surprising turns Wang has experienced since the virus was first discovered. Another? Suddenly, people with no background in biology, much less molecular biology, are asking him detailed questions about viruses.
“It’s surprising how suddenly the general public has become interested with sequencing,” he said. “Now, I have to explain (these things) to friends and family. That is something that was unexpected.”